Do you or someone you love have keratoconus? It may seem dire, but it doesn’t have to be. One of the most effective treatment options for people with progressive keratoconus is corneal cross-linking. Keep reading to learn more about why corneal cross-linking is a big deal!
What is Keratoconus?
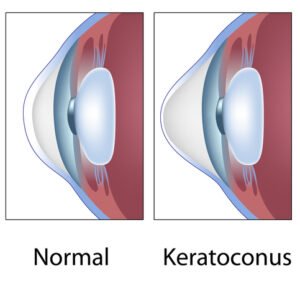
The cornea is the outer part of the front of the eye. This surface lets light into the lens, where it helps focus the eye. The cornea must be rounded to bend light to the lens and provide clear vision.
If you have keratoconus, your cornea is cone-shaped instead of gently rounded. This disfiguration makes it challenging to focus.
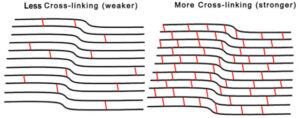
When you have keratoconus, collagen protein fibers in the eyes weaken. They won’t provide enough structural support to hold the cornea in place and create a rounded surface, necessary for seeing clearly.
You may have a sensitivity to glare and light if you have this condition. You’ll likely notice cloudy vision or focus that worsens as the disease progresses.
It may be challenging to drive at night. Many people with keratoconus need to change their glasses or contact lens prescription frequently.
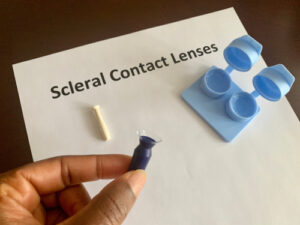
During the early stages, you may treat blurred vision with glasses or soft contacts. More severe cases may need gas-permeable or scleral contact lenses.
Some people get cornea transplants or corneal cross-linking to treat progressive or advanced stages of keratoconus.
What Factors Affect My Risk of Having Keratoconus?
No one knows the cause of keratoconus. However, here are some identified risk factors.
Around 1 in 10 people who have keratoconus have a parent who also has the condition. Having direct family members with the disease can increase your chances of developing keratoconus.
Some health conditions like Down syndrome and Ehlers-Danlos may also increase your likelihood of developing keratoconus.
People who regularly rub their eyes can increase their chances of the condition. Eye rubbing can also worsen keratoconus if you’ve already been diagnosed with it.
Retinitis pigmentosa can enhance your risk. Those with asthma or hay fever also have a higher likelihood of keratoconus. These conditions increase inflammation of the eye and may damage corneal tissue.

Keratoconus is most common among teenagers. Some children or people who are over age 30 develop the condition. It’s not common among individuals who are aged 40 and up.
What is Corneal Cross-Linking?
Corneal cross-linking is a procedure that can prevent keratoconus from worsening. It may not improve your vision, but it could stop it from degrading and preserve your remaining vision. This FDA-approved treatment is minimally invasive and takes around an hour to perform.
Before undergoing corneal cross-linking surgery, you will take a mild sedative. A Williamson Eye Center staff member will apply numbing eye drops to prevent pain during the procedure.
Because of these numbing eye drops, you should not feel any pain. Some people feel as if there is sand or grit between their eyes and lids.
Your eye doctor will apply liquid riboflavin drops to the corneal tissue. This vitamin B2 mixture strengthens the collagen fibers and is what allows the cross-linking reaction to take place.
The new cross-links provide structural support. Strengthening them can prevent the cornea from bulging further and distorting your sight.
You will lie still for about 30 minutes so the drops can absorb deep into the tissues. After, your eye doctor will apply a contact lens that will act as a bandage to protect the cornea while it heals. Follow their instructions on when to remove the lens.
Avoid rubbing your eyes for five days after the procedure. Wear sunglasses to protect yourself from sunlight.
You shouldn’t experience a great deal of pain after having corneal cross-linking, but some people feel discomfort. Use doctor-approved eye drops to reduce irritation and to prevent yourself from rubbing your eyes whenever possible.
You may have blurry vision for a few days after cross-linking. It can take up to 3 months for your eyes to heal and your sight to start improving. People who use glasses or contacts may need different prescriptions after the procedure.
What Are the Risks Associated With Corneal Cross-Linking?
As with any surgical procedure, corneal cross-linking does have potential risks and complications that can occur. This procedure can cause eye infections.
If you develop an eye infection, professional treatment should be able to address this issue.Eye pain and swelling may occur but should subside after a few days.
There may be damage to the epithelium or to the cornea during cross-linking. Blurred vision or other sight issues may continue after the surgery.
Many patients still require prescription glasses or contacts after cross-linking. The surgery can slow keratoconus, but it will not restore lost sight.
Having corneal cross-linking can stiffen your corneas and help you stop vision loss progression due to keratoconus.
Am I a Good Candidate for Corneal Cross-Linking?
The only way to know for sure if you may be a good candidate for corneal cross-linking is to talk to your eye doctor about it. They will consider your age and keratoconus progression.
They will also assess your corneal thickness. People who have thin corneal tissues (less than 400 microns) may not be candidates for the procedure.
People who had corneal stroma removed during penetrating keratoplasties or deep anterior lamellar keratoplasty cannot have corneal cross-linking. They do not have enough tissue to benefit from the riboflavin eye drops used during corneal cross-linking.
For patients with keratoconus, corneal cross-linking is one of the most successful treatment options available. With six convenient locations throughout Louisiana and a specialized Keratoconus Treatment Center in Baton Rouge, Williamson Eye Center makes it easy to determine if this treatment could be right for you.
Schedule a consultation with us in Baton Rouge, LA today!